HEALTHCARE CASE STUDY
Automating Clinical Note Summarization
Using Natural Language Processing to reduce clinician documentation time and improve care coordination.
The Client
Regional Healthcare Network
Industry: Healthcare
A network of hospitals and clinics seeking to reduce clinician burnout by addressing the growing burden of documentation while improving information exchange between providers.
The Challenge
The client was facing significant challenges with clinician burnout, with physicians spending hours daily on documentation. Clinical notes were lengthy, inconsistently structured, and critical information was often buried within verbose narratives, making it difficult to quickly extract key insights during care transitions.
- Physicians spending up to 2 hours daily on documentation alone.
- Inconsistent note structure making information retrieval difficult.
- Care coordination challenges during patient handoffs.
- Growing clinician burnout affecting retention and care quality.
Our AI-Powered Solution
Businesses Alliance developed an NLP-based clinical note summarization system that automatically extracts and organizes key information from free-text clinical documentation. Key components included:
- Medical Entity Recognition: Custom-trained NLP model to identify and extract critical medical entities such as diagnoses, medications, procedures, and lab values.
- Importance Classification: ML algorithm to prioritize and highlight the most clinically relevant information.
- Structured Summary Generation: System to convert unstructured notes into standardized, scannable formats with consistent sections.
- EMR Integration: Seamless integration with the existing Electronic Medical Record system.
- Progressive Learning: Feedback mechanism that allows the system to continuously improve based on clinician input.
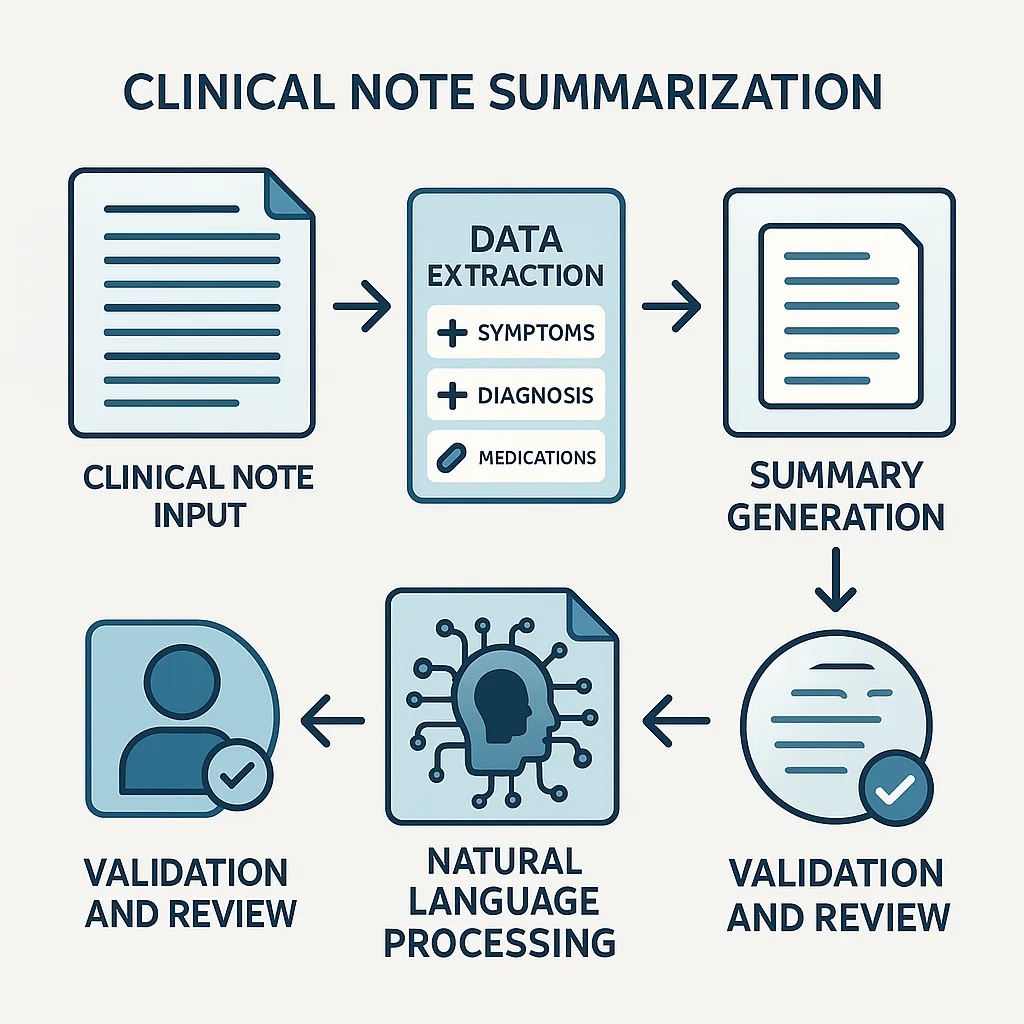
Illustration of the clinical note summarization process.
Implementation Journey
Phase 1: Discovery & Data Collection
Analyzed existing clinical documentation workflows, identified key information types, and collected anonymized training data. (Weeks 1-3)
Phase 2: Model Development & Training
Developed and trained specialized NLP models on medical terminology, built extraction and summarization algorithms. (Weeks 4-10)
Phase 3: Interface & Integration
Created user interfaces for clinician interaction, integrated with EMR APIs, and developed the feedback collection system. (Weeks 11-16)
Phase 4: Pilot & Optimization
Deployed with select departments, gathered feedback, refined algorithms, and improved accuracy before full rollout. (Weeks 17-24)
Quantifiable Results
Reduction in Documentation Time
Before vs. After Minutes/Patient
Improvement in Care Coordination Scores
Internal Satisfaction Survey
Increase in Clinician Satisfaction
Burnout Survey Scores